[ad_1]
Matthew Perry is opening up about his decades-long battle with addiction and how Jennifer Aniston was the friend who really stepped in and stepped in.
The revelations come in her upcoming memoir, “Friends, Lovers, and the Big Terrible Thing,” and an interview with Diane Sawyer that will air on ABC on Friday, Oct. 28.
In a sneak peek of Sawyer’s interview with Perry, the 53-year-old “Friends” star details her substance abuse issues like never before.
“Secrets kill you,” Perry said in the preview clip, obtained by E! news “Secrets kill people like me.”
 Jennifer Aniston and Matthew Perry on January 23, 1995 in Century City, California.Ron Galella Collection via Getty Images
Jennifer Aniston and Matthew Perry on January 23, 1995 in Century City, California.Ron Galella Collection via Getty Images
“At the time it should have been the toast of the city,” he added. “I was in a dark room meeting with drug dealers and completely alone.”
Sawyer lists “methadone, Xanax, full quart of vodka” as Perry’s drugs and drinks of choice, before adding “55 Vicodin a day.”
Later in the preview clip, Perry is asked about Aniston, who he calls Jenny, detailing a run-in the two had at the height of their addiction.
Sawyer quotes Aniston as saying, “We know you’re drinking.”
“Imagine how scary that was,” Perry replies.
Perry added that Aniston’s support was desperately needed in her recovery journey. “She was the one who came the most,” he said, adding, “I’m very grateful to her for that.”
[ad_2]
Source: https://news.google.com/__i/rss/rd/articles/CBMifGh0dHBzOi8vd3d3Lm5iY25ld3MuY29tL3BvcC1jdWx0dXJlL2NlbGVicml0eS9tYXR0aGV3LXBlcnJ5LXJlY2FsbHMtc2NhcnktY29uZnJvbnRhdGlvbi1qZW5uaWZlci1hbmlzdG9uLWFkZGljdGlvbi1yY25hNTM2NjXSAQA?oc=5 [ad_2]Methadone Clinic In My Area – Methadone Clinics New York – Methadone Clinics USA
The Senate officially confirmed Brett Kavanaugh as the next Supreme Court Justice on Saturday, Oct. 6. Several protestors in the public viewing gallery interrupted the vote, arguing someone accused of sexual assault should not hold such a position.
Alcohol’s Impact on Reporting Sexual Assault
Following Kavanaugh’s hearing, many women have come forward sharing their reasons for not reporting sexual assault by using the hashtag #WhyIDidntReport. Like Christine Blasey Ford, thousands of women mentioned drinking or underage drinking as a reason for not reporting.



In the second part of our series about the link between alcohol and sexual assault, we cover the barriers that alcohol presents in keeping survivors from reporting their assaults.

Did you miss part 1? Read it here: The No. 1 Date Rape Drug is 100% Legal .
The post Infographic: How Drinking Impacts Reporting Sexual Assault appeared first on Drug Rehab Options.
Methadone Clinic In My Area – Methadone Clinic NYC – Methadone Clinics USA
[ad_1]
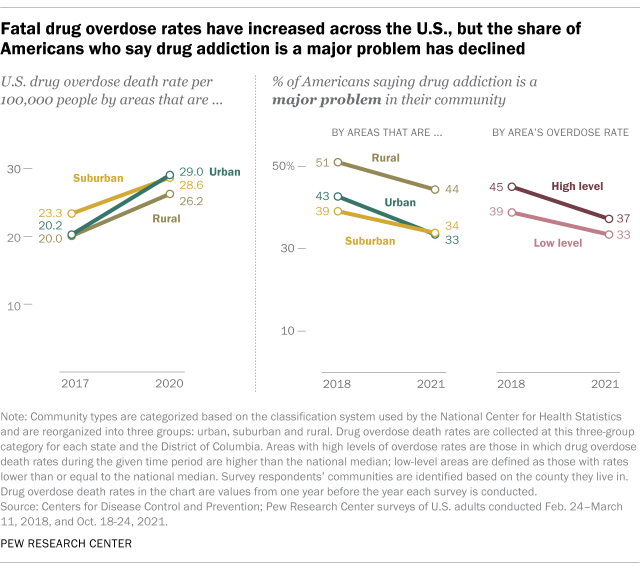
The share of Americans who see drug addiction as a “major problem” in their community has declined in recent years, even as drug overdose deaths in the United States have risen sharply. Public concern about addiction has fallen even in parts of the United States where drug overdose death rates have risen the most.

This Pew Research Center analysis examines changing public attitudes about drug addiction in the United States, including the communities that have been hardest hit by fatal drug overdoses in recent years.
The public opinion data cited here comes from two Pew Research Center surveys. The first was conducted from February 24 to March 11, 2018 among 6,251 US adults, and the second was conducted from October 18 to 24, 2021 among 9,676 US adults. All participants in these two surveys were members of the Center’s American Trends Panel (ATP), an online survey panel that is recruited through a national random sampling of residential addresses. That way, almost every American adult has a chance of being selected. Both surveys are weighted to be representative of the US adult population by gender, race, ethnicity, party affiliation, education and other categories. You can read more about ATP’s methodology, as well as the methodology for the 2018 and 2021 surveys.
The drug overdose death rates are taken from the Centers for Disease Control and Prevention’s WONDER database, specifically the database that shows the underlying causes of death from 1999 to 2020. The Center asked age-adjusted drug overdose death rates for 2017 and 2020 at three levels of urbanization—urban, suburban, and rural—for each state and the District of Columbia separately. While the CDC uses six levels of urbanization based on the National Center for Health Statistics’ classification system, the Center collapsed those six groups into three: urban, suburban, and rural, following the same methodology used in a 2018 report.
In addition to examining different levels of urbanization, we also grouped respondents into categories based on fatal drug overdose rates in their type of area (urban, suburban, or rural). We used respondents’ counties of residence to group them into the specified areas. One analysis groups respondents based on whether urban-level drug overdose death rates in their area were higher or lower than the national average in a given time period. Another groups the same respondents by whether the change in the drug overdose death rate in their area between 2017 and 2020 was greater than the average increase. Survey results may differ from previously published results due to differences in how urban, rural, and suburban classifications were defined.
Nearly 92,000 Americans died of drug overdoses in 2020, compared to about 70,000 in 2017, according to the Centers for Disease Control and Prevention (CDC). During the same period, the rate of fatal overdoses increased from 21.7 to 28.3 per 100,000 people.
Despite these increases, the share of Americans who say drug addiction is a major problem in their local community declined 7 percentage points in subsequent Pew Research Center surveys, from 42% in 2018 to 35% in 2021. And in an independent poll by the Center in early 2022, the fight against drug addiction ranked lowest among 18 priorities the president and Congress must address this year.
Fatal drug overdose rates rose in urban, suburban and rural areas of the country between 2017 and 2020. But the share of Americans who say drug addiction is a major problem declined in all three types of areas in the Center’s subsequent surveys. These declines ranged from 10 percentage points in urban areas (from 43% in 2018 to 33% in 2021) to 5 points in suburban areas (from 39% to 34%).
Public concern about drug addiction has declined even in areas with high levels of drug overdose deaths. In areas of the country with higher than average drug overdose death rates in 2017 and 2020, the share of Americans who say drug addiction is a major problem in their community decreased by 8 points between 2018 and 2021, from 45% to 37%.
This pattern is nearly identical in areas where drug overdose death rates increased more than the average increase between 2017 and 2020. 44% of Americans living in these areas said addiction to drugs was a significant problem in their community in 2018, but this share dropped. to 38% in 2021.
It’s unclear why public concern about drug addiction has waned in recent years, even in areas where overdose death rates have risen rapidly. The Center’s polls show that Americans have prioritized other issues, including the national economy, reducing health care costs and dealing with the coronavirus outbreak. The increase in overdose deaths may also be overshadowed, especially amid the high death toll attributed to the coronavirus outbreak (although, as of this month, far fewer see the virus as a major problem in the which the country faces).
Meltem Odabaş is a computational social scientist focused on data science at the Pew Research Center.
[ad_2]
Source: Concern over drug addiction eases even as fatal overdoses rise most in U.S.
Methadone Clinics In My Area – Methadone Clinic New York – Methadone Clinics USA
[ad_1]
When Owen Pelletier of Cowessess First Nation thinks back to her childhood, there are few happy memories.

“My parents suffered trauma and put him to sleep through drugs and alcohol and ended up abandoning our children and we experienced neglect, abuse and neglect,” he told Global News.
Pelletier recalled experiencing the same treatment in foster care, in addition to racism and discrimination.
“As far as I was concerned, I was the cozy little Indian. That was my title. That was my identity, the cozy little Indian, ”he said.
There was no relief at the school where Pelletier said he was harassed and despised.
Read more:
“Hope arrives”: The court resolves a step towards keeping more indigenous children out of foster care
The story continues under advertising
“You spend seven years in this type of environment, what do you think will happen to a person? You’ll get angry, ”he said, adding,“ If we don’t know the coping mechanisms, how to deal with it properly, we want to join the gangs and we want to smoke drugs and drink alcohol. ”
This is what happened to Pelletier.
He joined a gang, became addicted to drugs and alcohol, and eventually ended up in the Saskatoon and Regina correctional facilities.
A young native, he never understood the root cause of his struggles.
“Thirty-four years before the lady said, ‘You suffer abandonment and neglect.’
Read more:
Indigenous education experts applaud Ontario’s curricular changes and promote learning
Once Pelletier realized he was experiencing intergenerational trauma, he began to address it.
“My mother was sent to a residential school as a child. She experienced emotional, physical, mental and sexual abuse by caregivers there and therefore was never cured of it. He buried her deep inside. And drugs and alcohol, that’s how we treat them. That’s how we put pain to sleep, “he said.
The story continues under advertising
Pelletier has also been the victim of family fractures since the 1960s Scoop by the family’s father.
“Therefore, it is easy to establish this connection, how these intergenerational traumas are transmitted,” he added.
On Recovery Day and National Day of Truth and Reconciliation, Pelletier reflects on his past, his own recovery, and his “second chance at life.”
One of the barriers to recovery, for some, may be the stigma associated with addiction.
Read more:
Ontario celebrates the first National Day for Truth and Reconciliation
“Society puts this stigma and judgment on people, families, law enforcement, health care providers, everyone has a level of judgment and stigma towards people who use drugs, often thinking it’s their fault. hers, ”explained Louise Lemieux White, co-founder of Families for Addiction Recovery.
“We know that addiction is not a choice and it is a disease that can be treated and prevented and we hope that people can get the compassion and empathy they deserve and not be stigmatized,” White added.
Pelletier said another barrier to recovery may be lack of acceptance.
“Once we understood that we were given a bad hand and that we are not bad people, we were given a bad hand and we suffer traumas and that is why we try to put them to sleep through drugs and alcohol. Once we understand that, we can start breaking that pattern and start healing, ”he said.
The story continues under advertising
Ontario Associate Minister of Mental Health and Addictions Michael Tibollo, who will spend time with several Indigenous communities next month, said Canadians must respect what Indigenous people have gone through and “give them the tools to help -to improve their lives “.
Read more:
“A permanent symbol of colonization”: how the poor health of First Nations affects water
“There are amazing individuals in indigenous communities who have never had a chance to really shine. There are teachings of indigenous culture that are extremely useful in dealing with many of the mental health problems and addictions we have, ”said Tibollo.
As an inspiring and motivating speaker and father of three, Pelletier now devotes his time to providing positive guidance for Indigenous youth and helping them on the right path.
“There’s so much negativity where they come from, there’s so much drug and alcohol, both inside and outside of prison, and so it was for me,” he said. “Trauma, suffering, pain, pain … I have friends who are on the ground because of this lifestyle and don’t face it. So if you approach it, acknowledge it, accept it and start working and heal yourself … You will have a great life “.
© 2021 Global News, a division of Corus Entertainment Inc.
[ad_2]
Source: https://globalnews.ca/news/8234003/trauma-addiction-recovery-indigenous-first-nation/ [ad_2]Methadone Clinic Near Me – Methadone Clinic NYC – Methadone Clinics USA
[ad_1]

- Fentanyl stays in the brain’s opioid receptors longer than other opioids.
- If a patient is given one of the top fentanyl use disorder medications, they may experience severe withdrawal.
- Withdrawal symptoms can cause patients to relapse, interrupting recovery and putting their lives at risk.
For years, doctors and other medical caregivers have been required to become certified to prescribe a drug to patients with opioid use disorders to treat addiction and reduce overdose deaths.
The drug is U.S. Food and Drug Administration-approved buprenorphine, commonly known by one brand name, Suboxone. Taking it as prescribed is one of the most effective ways to treat patients and protect them from overdose.
Ideally, patients can start buprenorphine without experiencing severe withdrawal. If they used heroin or other opioids, they may need to wait 12 hours to a couple of days after their last use before taking the drug.
But with fentanyl, the wait is much longer. And if buprenorphine is started too soon, it can cause the patient to go into severe withdrawal and return to fentanyl use.
“I call fentanyl sticky”
Fentanyl stays in a person’s body, at mu opioid receptors in the brain, longer than other opioids.
“I call fentanyl sticky because it sticks to the receptors for so long,” said Dr. Mina “Mike” Kalfas, a board-certified addiction expert at the Travel Recovery Center in St. Elizabeth Healthcare in Northern Kentucky. “It’s just the nature of the drug. Each drug has its own unique action on the (mu opioid) receptor, and that’s unique to fentanyl.”
Kalfas began treating patients with Suboxone nearly 20 years ago, when the drug was new. Prescription painkiller abuse was on the rise in Kentucky, and heroin was coming onto the scene. He started with half a dozen Suboxone patients and has grown to about 250 at any given time to whom he prescribes the drug.

Now, most of them come to be treated for fentanyl addiction.
And Kalfas is seeing a new problem: Patients addicted to fentanyl are having to wait longer to start the medication regimen, he said. This means enduring days in retreat. Because if they are given buprenorphine too soon or at too high a dose, they can experience excruciating withdrawal, known medically as precipitated withdrawal.
Symptoms are so bad that people with opioid use disorder can relapse.
“The problem is, once they start retreating, they run,” Kalfas said. “They feel terrible, because withdrawal is what they fear the most.”
Fentanyl presents a unique public health challenge, treatment
It’s a situation that opioid addiction experts have known about for a few years, as fentanyl has overtaken heroin and been found in a number of other drugs of abuse.
Dr. Adam Bisaga, an addiction research specialist at Columbia University, noted in a 2019 report that replacing heroin use with non-pharmaceutical fentanyl “poses unique challenges for public health and treatment professionals “. He said doctors were reporting problems with patients experiencing delayed or precipitous withdrawal as they were induced with buprenorphine.
“New strategies to reduce mortality among opioid users are urgently needed,” Bisaga wrote. “Research programs must be established to quickly generate evidence to guide interventions targeting people affected by the influx of fentanyl.”

Kalfas, who is certified to treat up to 275 buprenorphine patients, said he has seen people with fentanyl in their system for days after their last use of the drug. Avoiding withdrawal when they start medication can be a struggle, she said, and if they don’t get through the wait, their desire to get help is destroyed and they’re back in danger of overdosing. It can be even worse to induce buprenorphine if it is too early to do so safely.
“Once I rush them severely enough, I’ve lost them,” Kalfas said. “I’ve lost their trust, I’ve pushed them back in their decision-making, and they tend to leave if they rush in here.”
Here’s what else Kalfas had to say about our questions about fentanyl
Answers have been edited for brevity and clarity.
Some patients report having trouble coming off fentanyl weeks after not using it. Is this possible?
Traveler: Yes. Norfentanil is a major metabolite of fentanyl that does not cause euphoria. It can remain in the receptors of the central nervous system for weeks. It is barely detectable.
Have you ever seen a patient take fentanyl pills by mistake, thinking it was a prescription drug?
traveler: Yes. For example, I had a guy come in and he said he took a “couple of oxys” for a back problem. I said, “That’s weird, there’s no oxycodone in the urine.” It’s all fentanyl. The patient was stunned.
Fake Flood Crime Lab:Hamilton County facilities often find fentanyl in fake prescription pills
Does Journey Recovery see a lot of people who primarily use fentanyl?
traveler: Yes. Every provider has new patient (buprenorphine) induction appointments every day.
If I have made an appointment to start treatment for opioid use disorder, how long will it take to get one?
traveler: Usually, if you call in the morning, we get you in the afternoon.
Do you think the treatment of addiction disorders needs to change?
traveler: Yes. The treatment must evolve with the evolution of use. When we saw heroin, we wanted to treat heroin. When we see fentanyl, we want to treat fentanyl. We are always playing catch. We need to treat addiction, not just addiction to a particular drug.
[ad_2]
Source: Fentanyl addiction is difficult to treat even with a drug expertMethadone Clinics Nearby – Methadone Clinics New York – Methadone Clinics USA
[ad_1]
source
[ad_2]Methadone Clinic Near Me – Methadone Clinic New York – Methadone Clinics USA
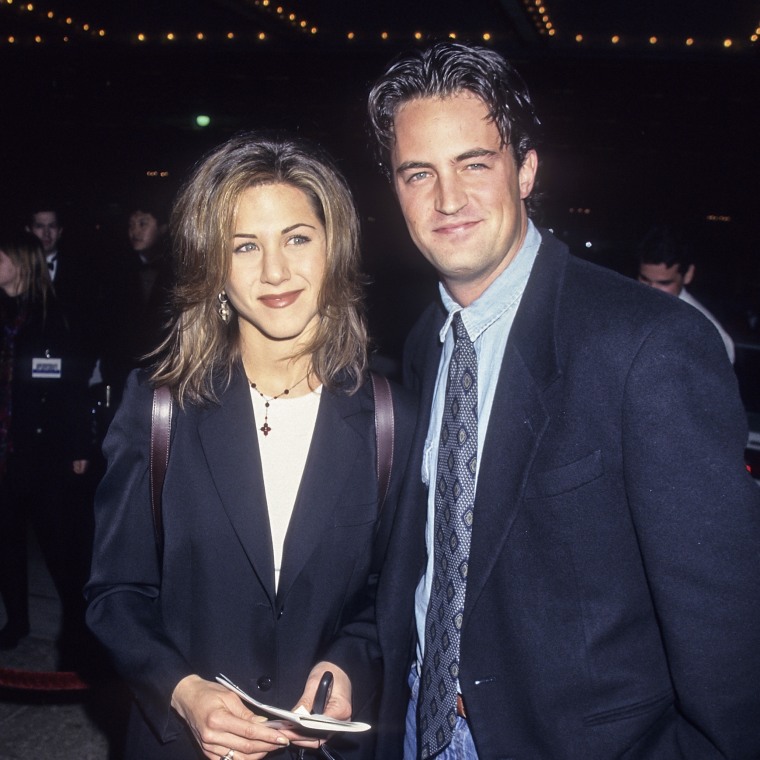 Jennifer Aniston and Matthew Perry on January 23, 1995 in Century City, California.Ron Galella Collection via Getty Images
Jennifer Aniston and Matthew Perry on January 23, 1995 in Century City, California.Ron Galella Collection via Getty Images