[ad_1]
In December, Marie, who lives in coastal Swampscott, Massachusetts, began having trouble breathing. Three days after Christmas, she woke up gasping for air and called 911.
“I was really scared,” Marie said later, her hand clutching her chest.
Marie, 63, was admitted to Salem Hospital, north of Boston. The staff treated her for chronic obstructive pulmonary disease, a lung disease. A doctor checked Marie the next day, said her oxygen levels looked fine, and told her she was ready to be discharged.
We do not use Marie’s last name because, like 1 in 9 inpatients, she has a history of drug or alcohol addiction. Disclosing a diagnosis like this can make it difficult to find housing, work, and even medical care in hospitals, where patients with addiction may be shunned.
But talking to the doctor that morning, Marie felt she had to disclose her other medical problem.
“‘I have to tell you something,'” Marie recalled. “‘I’m addicted to heroin. And I’m, like, starting to go into severe withdrawal. I literally can’t move. Please don’t let me go.'”
In many hospitals in Massachusetts and around the country, Marie would likely have been discharged anyway, still in the pain of withdrawal, perhaps with a list of local detox programs that could provide help.
Discharging a patient without specialized addiction care can mean missing a crucial opportunity to intervene and treat someone in the hospital. Most hospitals don’t have specialists who know how to treat addiction, and other doctors may not know what to do.
Hospitals often employ all kinds of providers who specialize in heart, lung, and kidney. But for patients with an addiction or a condition related to drug or alcohol use, few hospitals have a doctor, whether a doctor, nurse, therapist or social worker, who specializes in addiction medicine.
That absence is surprising at a time when overdose deaths in the U.S. have reached record highs, and research shows that patients are at greater risk of fatal overdose in the days or weeks after being discharged from a hospital
“They’re left on their own to figure it out, which unfortunately usually means starting over [drug] use it because it’s the only way to feel better,” said Liz Tadie, a registered nurse in addiction care.
In the fall of 2020, Tadie was hired to launch a new approach at Salem Hospital with a $320,000 federal grant. Tadie created what is known as an “addiction consultation service”. The team included Tadie, a patient case manager, and three recovery coaches, who drew on their experiences with addiction to advocate for patients and help them navigate treatment options.
After Marie asked her doctor to let her stay in the hospital, she called Tadie for a bedside consultation.
Tadie started out on methadone, a drug to treat opioid addiction. Although many patients do well on this drug, it didn’t help Marie, so Tadie switched her to buprenorphine, with better results. After a few more days, Marie was discharged and continued to take buprenorphine.
Marie also continued to see Tadie for outpatient treatment and turned to her for support and reassurance: “Like, that I wouldn’t be alone,” Marie said. “That I wouldn’t have to call a dealer again, that I could delete the number. I want to get back to my life. I just feel grateful.”
Tadie helped spread the word among Salem’s clinical staff about the expertise she offered and how she could help patients. Success stories like Marie’s helped make the case for addiction medicine and helped unravel decades of misinformation, discrimination and ignorance about addiction patients and their treatment options.
The little amount of training that doctors and nurses receive is often not helpful.
“A lot of the facts are outdated,” Tadie said. “And people are trained to use stigmatizing language, words like ‘addict’ and ‘substance abuse.’
Tadie gently corrected the doctors at Salem Hospital, who, for example, thought they weren’t allowed to start patients on methadone at the hospital.
“Sometimes I would recommend a dose and someone would talk me back,” Tadie said. But “we got to know the doctors at the hospital, and over time they said, ‘OK, we can trust you.’ We will follow your recommendations.”
Other members of Tadie’s team have struggled to find their place in the hospital hierarchy.
David Cave, one of Salem’s recovery coaches, is often the first person to speak to patients who come to the emergency room in withdrawal. It tries to help doctors and nurses understand what patients are going through and help them navigate their care. “I’m probably punching above my weight every time I try to talk to a doctor or physician,” Cave said. “They don’t see letters after my name. It can be a little tough.”
Calling addiction a specialty and hiring people with specific training is changing the culture at Salem Hospital, said social worker Jean Monahan-Doherty. “Finally, there was some recognition throughout the institution that this was a complex medical condition that needed specialist attention,” Monahan-Doherty said. “People are dying. This is a terminal illness unless it is treated.”
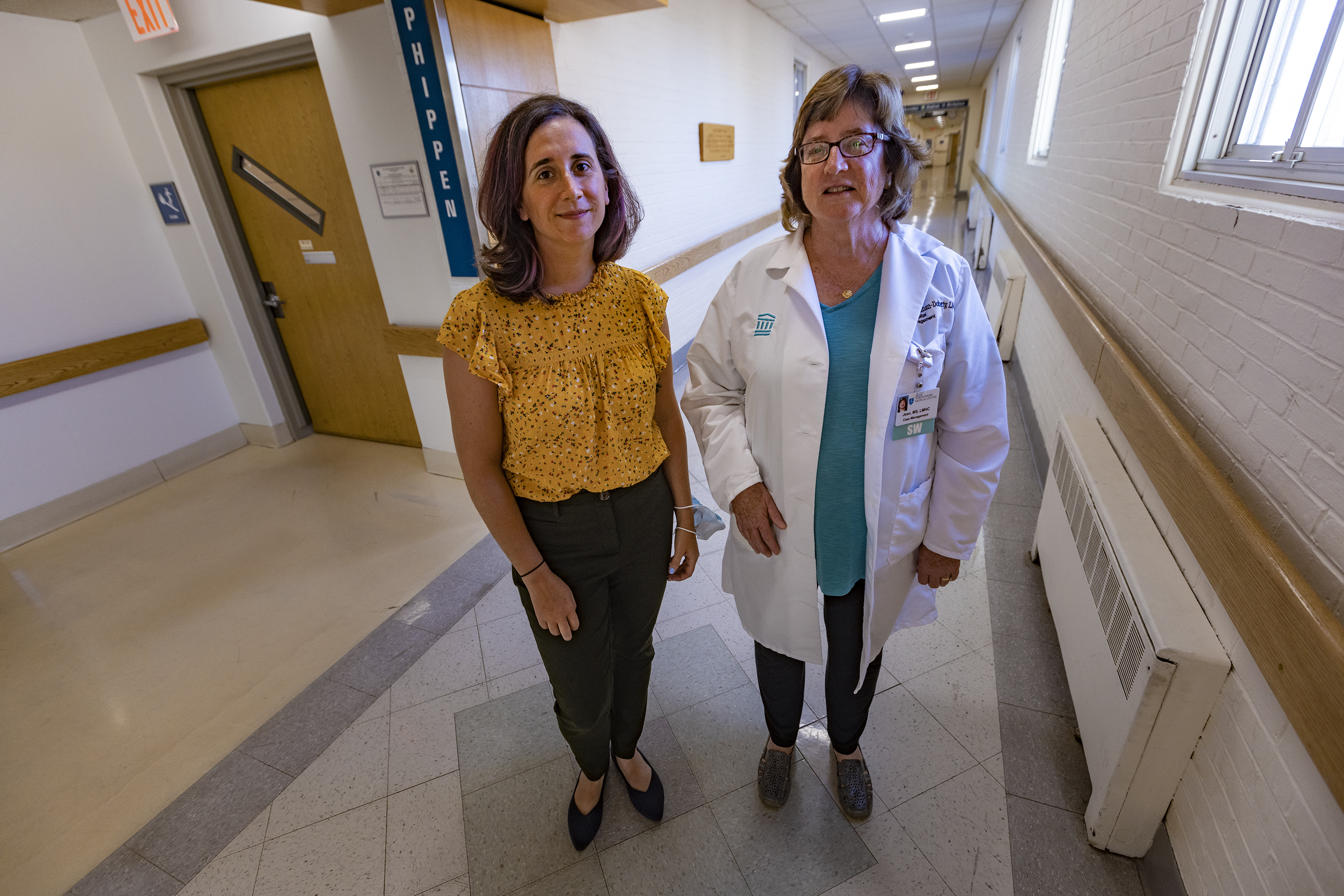 Liz Tadie (left) was the director of substance use disorder services at Salem Hospital in North Boston. Jean Monahan-Doherty (right), a social worker at the hospital, says: “Finally there was some recognition throughout the institution that this was a complex medical condition that needed specialist attention.” Tadie is starting a job at another hospital, but Salem Hospital leaders say the program will continue.(Jesse Costa/WBUR)
Liz Tadie (left) was the director of substance use disorder services at Salem Hospital in North Boston. Jean Monahan-Doherty (right), a social worker at the hospital, says: “Finally there was some recognition throughout the institution that this was a complex medical condition that needed specialist attention.” Tadie is starting a job at another hospital, but Salem Hospital leaders say the program will continue.(Jesse Costa/WBUR)
This approach to treating addiction is winning over some employees at Salem Hospital, but not all.
“Sometimes you hear an attitude of, ‘Why are you putting all this effort into this patient?’ They won’t get better.’ Well, how do we know?” Monahan Doherty said. “If a patient comes in with diabetes, we don’t say, ‘OK, they’ve been taught this once and it didn’t work, so we’re not going to support them again.'” .
Despite lingering reservations among some Salem doctors, demand for addiction services is high. Many days, Tadie and his team have been overwhelmed with referrals.
Four other Massachusetts hospitals added addiction specialists in the past three years through federal funding from the HEALing Communities study. The project is paying for a wide range of strategies in several states to help determine the most effective ways to reduce drug overdose deaths. They include mobile treatment clinics; street outreach teams; distribution of naloxone, a drug that can reverse an opioid overdose; travel to treatment sites; and multilingual public awareness campaigns.
It’s a new field, so finding staff members with the right certifications can be a challenge. Some hospital leaders say they are concerned about the costs of addiction treatment and fear they will lose money on the efforts. Some physicians report that they do not want to initiate drug treatment while patients are in the hospital because they do not know where to refer patients after discharge, whether to outpatient follow-up or a residential program. To address follow-up care, Salem Hospital started what is known as a “bridge clinic,” which provides outpatient care.
Dr. Honora Englander, a national leader in specialist addiction programs, said the federal government could support the creation of more addiction consultation services by offering financial incentives or penalties to hospitals that do not accept them.
At Salem Hospital, some staff members worry about the program’s future. Tadie is starting a new job at another hospital and the federal grant ended on June 30. But Salem Hospital leaders say they are committed to continuing the program and the service will continue.
This story is part of a partnership that includes WBUR, NPR and KHN.
marthab@wbur.org, @mbebinger
Related topics
Contact us Submit a story tip
[ad_2]
Source: https://news.google.com/__i/rss/rd/articles/CBMiWGh0dHBzOi8va2huLm9yZy9uZXdzL2FydGljbGUvaG9zcGl0YWxzLWhhdmUtYmVlbi1zbG93LXRvLWJyaW5nLW9uLWFkZGljdGlvbi1zcGVjaWFsaXN0cy_SAVxodHRwczovL2tobi5vcmcvbmV3cy9hcnRpY2xlL2hvc3BpdGFscy1oYXZlLWJlZW4tc2xvdy10by1icmluZy1vbi1hZGRpY3Rpb24tc3BlY2lhbGlzdHMvYW1wLw?oc=5
Methadone Clinics Nearby – Methadone Clinic NYC – Methadone Clinics USA















